Sometimes one adrenaline autoinjector might not be enough
Sometimes one adrenaline autoinjector might not be enough
Allergic disease impairs patients’ quality of life and, may in some instances cause life-threatening reactions, also called anaphylaxis. Common triggers of anaphylaxis are food in children and food, drugs, or insects (bee/wasp) in adults. Typically, anaphylaxis presents within minutes (2-20) following contact with the substance you are allergic to. Frequently, the reaction starts with wheals and itch. Swelling of the face, hands, or feet can also occur. Patients can sometimes develop shortness of breath, dizziness, vomiting, diarrhea or stomach pains as well. If you are lucky, the reaction will resolve without it getting worse. However, allergic reactions can also become more severe, causing acute shortness of breath, a drop in blood pressure, loss of consciousness, or even death.
Adrenaline is the recommended drug to treat anaphylaxis. It can be given intramuscularly (i.m.) or intravenously (i.v.). The i.v. administration may have side effects and must be performed by an experienced doctor. On the other hand, the i.m. injection into the outer side of the upper leg is much safer and can be performed by a lay person before professional medical treatment is available. Indeed adrenaline autoinjectors (AAIs) were developed for this purpose. AAIs are more reliable, faster, and easier to use than normal syringes for someone without medical training. Thus, medical guidelines worldwide recommend that patients with a history of anaphylaxis are prescribed anAAI that they should always carry with them.
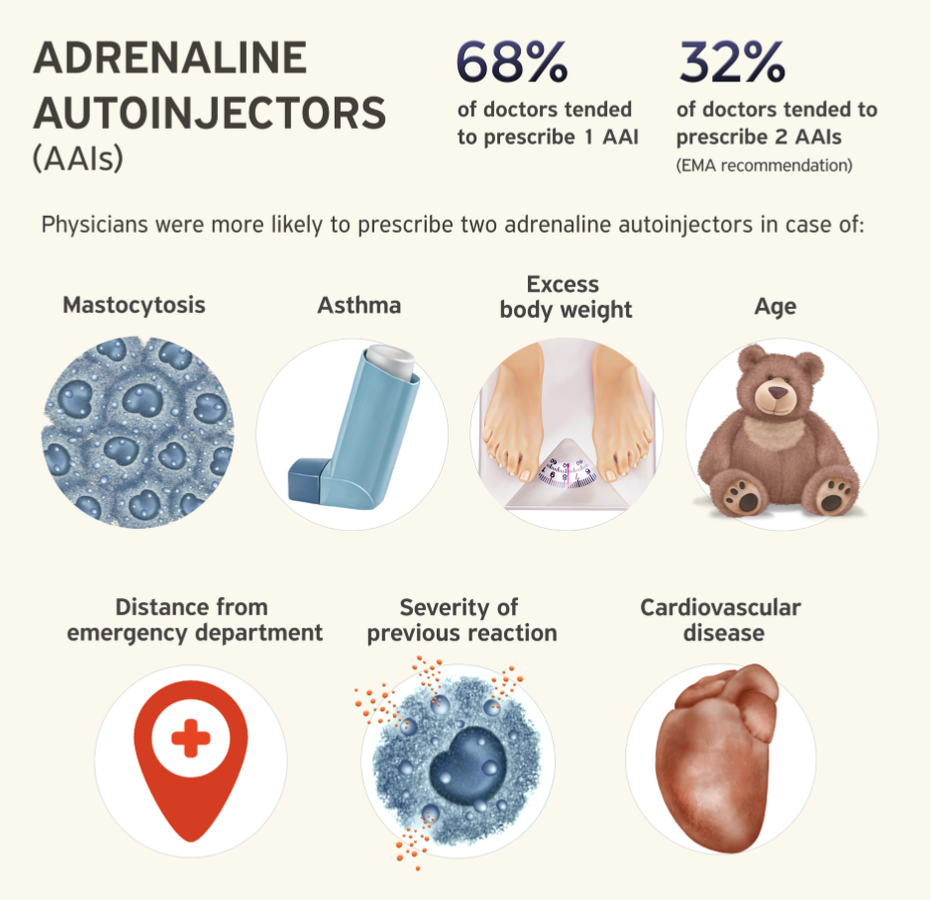
The number of AAIs that should be prescribed per patient is an open question. Having more than one per patient might be useful in some circumstances. For example, the AAI may accidentally be used incorrectly, or one standard dose might be not enough for every patient, thus often multiple AAIs are prescribed. However, AAIs are expensive, expire within several months, and must be carried at all times. The guidelines of the European Academy of Allergy and Clinical Immunology (EAACI) have defined circumstances in which a patient should be prescribed more than one AAI. These are as follows: unstable or moderate-to-severe persistent asthma and a food allergy, mast cell diseases and elevated baseline tryptase,[1] lack of access to emergency medical services, a previous reaction requiring more than one dose of adrenaline, or near-fatal anaphylaxis, and/or if the patient has been prescribed an AAI which has a much lower dose of adrenaline than that adequate for their weight. The European Medical Agency recommends the prescription of two AAIs for all patients.
We carried out a study to examine how experts from specialized allergy centers follow these recommendations in their daily practice regarding the number of AAI prescribed and which factors influence their decisions. We asked 26 allergy experts who attended the 4th international anaphylaxis conference of Network for Online Registration of Anaphylaxis (NORA e.V.) held together with the meeting for the EAACI Task force on Clinical epidemiology of anaphylaxis in April 2019 in Berlin, about their prescription habits. Most allergy doctors (68%) usually prescribed one AAI, and 32% prescribed usually two or more AAIs. Respondents tended to prescribe more than one AAI if the patient was a child or had a history of a severe anaphylaxis. The trigger of anaphylaxis (food vs. insect) was not an important factor, whereas mast cell disease, increased body weight, asthma, or cardiovascular diseases as comorbidities were. Also, if the patients lived far from the emergency department, they were more likely to be prescribed two AAIs. In addition, the regulatory and reimbursement aspects appear to influence approximately half of the experts.
Our preliminary data shows that, even among specialists, different opinions on how many AAIs should be prescribed exist. Further studies are needed to identify which patients benefit from the second AAI the most, and which factors influence physicians’ decisions on the number of AAIs prescribed. Also, efforts to lower the costs of AAIs and extend their half-life should be made to increase their availability.
https://pubmed.ncbi.nlm.nih.gov/32426107/
[1] Mast cell disease is a rare disorder with increased risk for severe anaphylaxis, and tryptase is a laboratory parameter associated with mast cell disease.